By Ken Kleinberg, Practice Lead, Innovative Technologies

There has been a tremendous amount written about the value of Health Information Exchanges (HIEs) in moving and making clinical and financial/benefit information available where it’s needed to improve decision making. Similarly, there’s been much written about challenges with HIEs, especially around interoperability standards, patient identity matching, sustainable business models, and a framework of trust. What’s often not discussed enough is how HIEs can best be integrated into provider workflow, for if this is not handled well, the benefits of an HIE may not be fully realized.
Three Scenarios
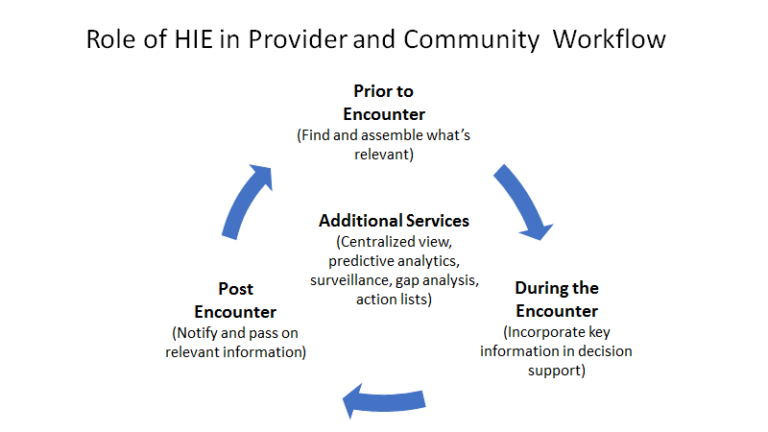
Consider three scenarios: What can be done preemptively before a patient encounter; what can occur during the encounter; and what would be valuable post-encounter. To make this more concrete, we’ll use medication therapy management (MTM) as an example.
Prior to a Patient Encounter: Once its determined that a patient will be seen, there is value in collecting historical and current information about the patient and assembling it in a way that will be most useful during the encounter. This includes what past medications the patient has taken (and whether they have been successful or not), lab and imaging test results, info from referrals, benefits and claims information, etc.
Since it’s not always clear where the patient received past treatments and there could be some delays obtaining the records, it’s best that this discovery starts well in advance of the actual visit. The search could be quite extensive if the patient has multiple chronic conditions, lived in multiple locations, had many providers, or different insurance companies. This discovery step is best carried out by the physician’s clinical staff, although physicians should develop profiles of the types of info they typically need to see for the kind of visit that will occur. Lots of great work is being done to support discovery and key use cases involving FHIR-based data exchange.
Hopefully, the HIE in use has the needed connectivity and search capabilities and the EHR has the ability to accept the information into a longitudinal record. Clinical Document Architecture (CDA) and Continuity of Care Documents (CCDs) were meant to address such needs, but EHRs have proven to not be fully up to the task of parsing out the necessary information for inclusion into the EHR. Unstructured data such as narratives present additional challenges – use of Natural Language Processing (NLP) can assist here in making that information more structured.
During the Encounter: There is no doubt that time is a key factor in patient encounters, and the few minutes that the physician has available should not be spent searching for information or hunting within CCDs. In the best case, relevant information prior to the encounter has already been incorporated into the EHR, and the workflow/decision support for diagnosis, ordering, etc., takes that information into account. More often, the interface between the EHR and the HIE is in the form of a notification or link on the EHR screen to alert the physician that information is available from outside sources. Mechanisms such as use of blinking or different colors can be employed to draw the necessary attention. The least efficient approach is for the physician to proactively search for information, which can be even more challenging if they need to leave the EHR to log-in to the HIE or re-enter information into their EHR.
After the Encounter: HIEs can play a valuable role in passing information and referrals to other systems and stakeholders – the more pre-configured the system is to carry out these steps for common occurrences the less onerous for the clinicians. A notification to the patient’s PCP that medications have changed is crucial, as this is a common place for challenges to occur as the patient adjusts to the new regime. For MTM, information has to flow to additional care professionals involved in therapy dispensing, administration, monitoring, coaching, etc. Reporting to registries (e.g., for cancer care) via the HIE is also a function that can be automated. A challenge with notifying others is ensuring they are not overwhelmed with low-priority or irrelevant alerts.
Distributed or Centralized Services
An emerging opportunity for HIEs is in providing services such as surveillance and analytics, not just data and notifications. These can help to close the loop for all three scenarios above and identify gaps in support of payer and provider goals of population health management (PHM).
For example, an HIE could distribute an object or run an algorithm to predict which patients were at greatest risk for certain conditions like diabetes or heart disease; then determine and collect the types of information that would be most relevant to prepare for these encounters. During the encounter, the system would suggest which medications and therapy approaches would be most relevant. At discharge, the system could make predictions and help with recommended steps to improve outcomes by tapping into the extended care network for follow-up and periodic tests.
Such algorithms would take advantage of the connectivity of the HIE with the various organizations and their (EHR) systems via APIs. If parties can agree, they could feed a centralized approach where the analysis capability would be made available to all in the network. Organizations like SHEIC can provide a rallying point for service distribution and new HIE revenue streams.
In our MTM example, the HIE could function like a coordination hub – connecting stakeholders that include the providers, patients, pharmacists (including specialty, hospital-based, and community retail), post-acute care, payers and others with a consistent, comprehensive, and reconciled view of medications for a patient. Information such as fill-information from the pharmacy could assist in understanding and improving adherence. Patients could annotate the meds list with what they may have purchased over the counter (OTC) with cash. Payers could provide more effective care/case management and help improve quality. Many HIEs are making progress with payer involvement and incentives for information sharing, such as efforts by the Michigan Health Information Network (MiHIN), Blue Cross Blue Shield of Michigan, and participating stakeholders.
What Can the Industry Do?
Data and analytics can only help if accessed and used. Industry efforts should therefore include improving workflow integration with key stakeholders. For providers, this includes decreasing manual prep time before encounters, having information and advice ready and integrated at the point of care, and ensuring that follow-on information sharing and surveillance steps are being taken without relying on manual steps. Including participation of pharmacists, payers, and other stakeholders beyond provider-to-provider interaction may be broader than the original vision of HIEs, but that’s what’s needed. It is going to make a difference.




